
For multi-location audiology clinics, revenue growth is closely tied to how effectively your team manages billing and collections. From understanding current coding and reimbursement requirements to maintaining consistent documentation and preventing denied claims, billing accuracy plays a critical role in keeping revenue predictable at scale, especially for multi-location clinics, who must manage finances at scale.
This blog breaks down key guidelines and best practices, helping multi-location hearing clinics leverage technology to simplify processes, reduce errors, and improve overall collections.
Why Audiology Billing Guidelines Can Get Hard at Scale

Accurate billing and timely collections are essential to maintaining healthy revenue and cash flow. As multi-location hearing clinics expand, billing processes become significantly more complex, introducing new operational, financial, and compliance challenges that can directly impact profitability.
Hearing care clinic networks must manage varying payer requirements, state-specific rules, and inconsistent documentation practices across sites. What works well in a single or few clinics often breaks down at scale, leading to coding errors, denied claims, delayed reimbursements, and increased administrative burden. Without standardized processes and clear oversight, even small inconsistencies can result in lost revenue.
Compounding these challenges, Medicaid and other insurance companies require Current Procedural Terminology (CPT) codes to be submitted for each service, as outlined by the American Medical Association. Unfortunately, each insurance company follows different rules, so there’s not a one-size-fits-all protocol when it comes to billing and medical coding. Your clinics must understand (and follow) the various rules and guidelines for each specific scenario.
Core Billing Challenges for Multi-Location Hearing Clinics

As hearing clinics expand, billing challenges often multiply rather than scale smoothly. Managing billing across multiple locations introduces inconsistencies that can negatively impact reimbursement, compliance, and operational efficiency. Therefore, it’s essential to have all staff at all locations follow proper audiology billing guidelines.
To accomplish this:
- Ensure Consistent Coding and Documentation Across Locations
Set up the proper technologies, workflows, and support to ensure that all staff code and document services properly. Inconsistent or inaccurate audiology billing codes often lead to insurance claim denials and delayed payments, which can negatively impact your practice’s collections – and bottom line. - Train Your Staff
Staff training variability can lead to major problems in your billing practices. Follow consistent training protocols in all locations, so staff across the enterprise understand the proper steps for billing, collections, and insurance reimbursement. Everyone should be following the same consistent practices across all your clinic locations, and that starts with standardizing your training protocols. - Navigate Payer Rules by State
One of the most complex aspects of audiology billing and collection is that payer rules vary by state. All employees must understand how to navigate this, with oversight across all clinic locations to ensure that this important task is being properly managed. If claims are submitted incorrectly, they’ll be denied, delaying payment collections for your clinic. At scale, this can result in significant cash-flow problems for your operation. - Optimize and Standardize Your Processes
Poor coordination and manual workloads can exacerbate challenges for your clinic. For instance, manual processes make it extremely difficult to get a comprehensive view of your enterprise’s finances, track trends, and identify issues. Manual processes also make it challenging to determine whether employees are following best practice workflows in every location – and to flag individuals that are deviating from the proper action.
U.S. Billing Basics Every Clinic Must Get Right
Your team must follow specific billing and insurance rules and regulations for the U.S. (and any other countries you serve). It’s essential that your team understands and follows proper claim formats, so claims are complete and accurate (with proper billing codes).
In the U.S., clinic staff must understand and apply Current Procedural Terminology (CPT) codes, coding services correctly for faster reimbursements and less risk of claim denials. There are different codes for various services. A common real-world scenario that affects approval rates is the binaural vs monaural HCPCS "v-codes" code selection. Some payers require two monaural lines instead of a single binaural line in some cases. For example, UnitedHealthcare’s exchange reimbursement policy says monaural hearing aids should be billed with LT or RT (not RTLT on one line), and if both ears are billed as monaural, they should be on separate claim lines. Billing incorrectly may cause a reimbursement delay or rejection. Educate staff about how to use CPT codes, emphasizing the importance of accuracy to get faster payments and avoid the administrative burden of resubmitting denied claims. For the most up-to-date list of code categories, rely on official websites like CMS.gov (Centers for Medicare & Medicaid Services).
It's also important to understand the International Classification of Diseases (ICD) codes, specifically ICD-10 codes, which are used to classify diagnoses, diseases, and health conditions. Recently, the ICD-10 codes changed to integrate more seamlessly with electronic health records (EHR) and other data systems. Your staff must use the updated codes – plus new features like extension codes and cluster coding – to document conditions like hearing loss, tinnitus, and ear infections.
How Technology Simplifies Billing at Scale
For multi-location audiology organizations, billing is not simply an operational task—it is a system-level discipline. As scale increases, so do the risks associated with inconsistency, manual work, and limited visibility. A secure, cloud-based audiology Practice Management Software (PMS) becomes essential for maintaining control, accuracy, and efficiency across the enterprise.

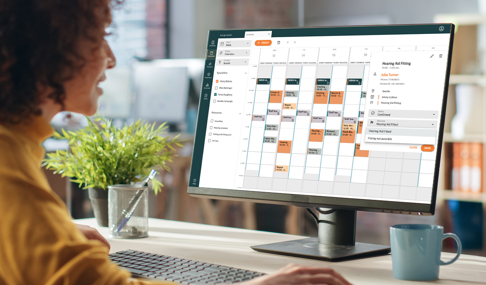
Auditdata’s PMS, Manage is designed for multi-location audiology clinics with standardized workflows and processes that guide staff through proper action sequences, ensuring that every employee – across every clinic – is following best practice protocols. Notably, Manage helps multi-location clinics:
- Standardize and Automate Processes
Use Manage to set up billing workflows that guide employees through a pre-determined sequence of tasks. This helps ensure consistent efforts across all clinic locations. Use shared templates so every clinic sends the same professional documents with the right fields and branding.
- Streamline Billing Efforts
Turn approved quotes into invoices in one click, standardize paperwork across locations, and ensure every invoice is tied to the right appointment. Doing these make reconciliation faster and reporting more dependable. Turn approved quotes into invoices in one click, standardize paperwork across locations, and ensure every invoice is tied to the right appointment. Doing this makes reconciliation faster and reporting more dependable. Another helpful feature is the environment settings in Manage, which allow you to personalize custom field configurations and mandatory fields to meet your organization’s needs and preferences. This helps ensure staff collect all required patient and clinical information accurately the first time, reducing the need to follow up later for missing details. You can choose exactly what information is needed to support a smooth billing/claims experience. Additionally, you can make those fields mandatory, so staff are prompted to complete them before moving forward. This ensures consistency, improves documentation quality, and helps avoid reimbursement hiccups.
- Customize Billing and Payments per Region
Manage guides employees through complex billing and insurance rules for the U.S., which vary by payer and geography. Manage helps your team provide necessary documentation, submit complete claims, reduce denials, boost efficiencies, and accelerate collections. - Make the CMS-1500 Claim Less Intimidating
The embedded CMS-1500 form has been broken down into four distinct sections to ensure seamless and efficient claims submissions directly from the patient sale screen. Using Manage for this task makes the CMS-1500 claim less imposing, ensures higher data entry quality, and makes training easier for new staff. Once the 835 is ready later this year, Manage will have the upgraded capability necessary to meet these new requirements.
- Boost Efficiency, Consistency, and Accuracy
Streamline operations across all clinic locations. Eliminate manual work and redundancies. Ensure consistent processes across each location in your network. Automate time-consuming tasks and reduce administrative burdens. Manage helps your team work smarter and more efficiently.
- Get a Holistic View Across Your Practice
One of Manage’s biggest benefits is the ability to collect and analyze data across your multi-location practice. As a result, you can easily track payments, spot trends, and identify (and fix) any problems across your network. Manage can provide data across the network and drill down by location or employee.
Explore the Billing Flow in Auditdata Manage
Get a clear, step by step view of billing in Auditdata Manage, from pre billing to reporting.

Documentation & Compliance: The Non-Negotiables
The key to receiving maximum reimbursement for your audiology services is the thoroughness and accuracy of your documentation. This includes proper coding and explanations for any audiology services, tests, diagnoses, and solutions, such as hearing aids.

Your documentation should include the reason for appointment visits, services provided, tests conducted, diagnoses made, solutions recommended, with proper code categories.
Make sure your employees:
- Know What to Document
U.S. audiology billing guidelines require careful documentation, including accurate CPT (procedure) and ICD-10 codes (diagnosis) codes. Additionally, audiology clinics must adhere to payer rules, which can vary by insurance companies and geographies. - Understand the Common Causes of Denials
Insurance denials are frequently due to common – and preventable – issues, such as patient registration errors (like the wrong DOB or misspelled name), coding mistakes (like using the wrong audiology billing codes), lack of proper pre-authorization, etc. Standardizing processes across all your clinic locations can help prevent these issues for faster reimbursements, fewer denials, and less need for time-consuming resubmissions. - Remember that Ethical Billing = Revenue Protection
Your team must always practice ethical billing, ensuring that their processes are transparent and accurate. As part of these efforts, employees must keep proper documentation about each patient’s medical history, diagnoses, services rendered, rationale for specific services, proper coding, etc.
Don't Miss Out On the Latest Insights On Audiology
Sign up today to receive exciting updates, tips, and the latest newsletters from Auditdata.
Other Blogs You Might Enjoy

Cybersecurity: Be Prepared – Not Scared: Strengthening Cybersecurity in Hearing Practices
While cybersecurity has become a pressing business issue, many audiology practices don’t have the necessary security measures in place to protect confidential data – including patients’ healthcare and financial information. Does yours?

Best Practices in Audiometry: Achieving Accurate and Consistent Results
Audiometric assessments play a crucial role in diagnosing and managing hearing disorders, making it essential to ensure that the results obtained are both accurate and consistent. This article explores the best practices in audiometry, offering a comprehensive guide to optimize the assessment process and enhance the reliability of outcomes.
9 Proven Tips to Improve Time Management in Hearing Practices
Time management skills in healthcare are critical because your staff is dealing with people’s well-being. In audiology, you’re always busy, and must work diligently and continuously to provide exceptional care and outstanding customer service. This blog outlines 9 proven tips to improve your time management skills and make the most of each day.